Frailty Matters
A Growing Health System Challenge
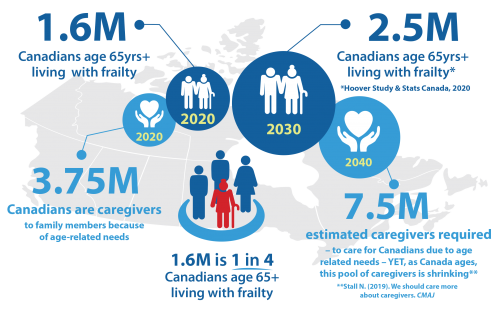
The burden of frailty in Canada is steadily growing. Today over 1.6 million Canadians are medically frail. And in 10 years, well over two million Canadians may be living with frailty. There are 3.75 million caregivers in Canada caring for an older adult (aged 65 and over) with a long term health problem, disability or age-related condition.
Frailty is also linked to higher consumption of healthcare resources. Of the $220 billion spent on healthcare annually in Canada (11% of GDP), 46% is spent on people over 65 years old, although they are only 16% of the population. The operating costs to care for the 7% of Canadians over the age of 65 that are living in long term care homes is $31 billion dollars.


Older Canadians living with frailty are over-represented in all parts of the healthcare system: primary care, community and residential care, acute care and end-of-life care. This growing population is both under-recognized and under-served, challenging the healthcare system to improve the quality and quantity of care delivered.
Currently, we have little evidence to guide the care of older adults living with frailty. We don’t know if current therapies are beneficial or cause harm, are cost-effective or waste scarce healthcare resources.
As well, the healthcare system is ill equipped to deal with frailty:
- Healthcare systems are organized to manage illness based on single body systems and diseases, not the complex multi-system problems of those living with frailty.
- Frailty is poorly understood, pervasively under-recognized, and under-appreciated by healthcare professionals and the public.
- Few healthcare professionals have expertise in caring for older adults living with frailty.
- Poor system integration causes poor outcomes for older adults living with frailty.
“Without evidence, aggressive and expensive technologies are often overused without improvement in outcomes, causing undue suffering to patients, undue distress to their families, caregivers and health care practitioners, and wasted health care resources.”
— CFN Scientific Director Dr. John Muscedere
Research on Aging, Policies and Practice. (June 2018). A profile of caregivers of older adults (65+). [Website] https://rapp.ualberta.ca/wp-content/uploads/sites/49/2018/09/Profile-of-Carers-of-Older-Adults-65-Infographic_2018-06-20.pdf
Infographic – Canadians over 65
- Statistics Canada. 2019. The Daily, Monday, September 30, 2019. Canada’s population estimates: Age and sex, July 1, 2019. Component of Statistics Canada catalogue no. 11-001-X Ottawa.
- Canadian Institute for Health Information. National Health Expenditure Trends, 1975 to 2019. Ottawa, ON: CIHI; 2019.
Infographic – LTC
- BCMJ, vol. 54 , No. 9 , November 2012 , Pages 450
- Statistics Canada. 2018. Health Reports. Transitions to long-term and residential care among older Canadians. Statistics Canada catalogue no. 82-003-XOttawa.
- Ontario Long Term Care Association 2019. This is Long-Term Care 2019. Toronto, Ontario: Ontario Long Term Care Association. © 2019 Ontario Long Term Care Association
- Sizing Up the Challenge: Meeting the Demand for Long-Term Care in Canada. Ottawa: The Conference Board of Canada, 2017.
